Pilot Grant Scholars and ESIs in San Francisco!
Check out the abstracts and poster gallery featuring our Pilot Grant Scholars and Early-Stage Investigators, some of whom attended and presented at the HEAN Annual Meeting in San Francisco, California!
-
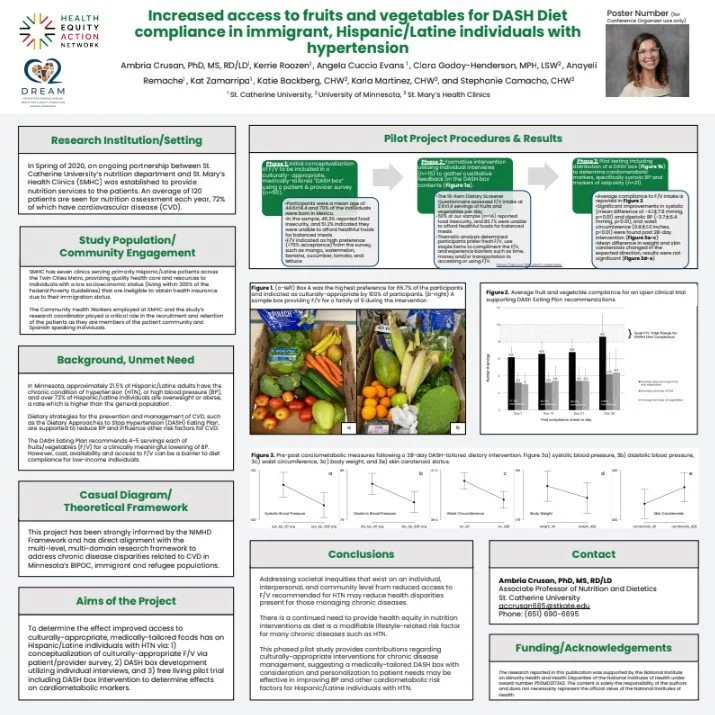
Ambria Crusan, Increased access to fruits and vegetables for DASH Diet compliance in immigrant, Hispanic/Latine individuals with hypertension
Purpose: The Dietary Approaches to Stop Hypertension (DASH) eating plan, a nutrition intervention for hypertension (HTN), fails to consider barriers to fruit and vegetable (F/V) consumption. This project aims to determine the effect improved access to culturally-appropriate, medically-tailored foods has on Hispanic/Latine individuals with HTN via: 1) conceptualization of culturally-appropriate F/V via patient/provider survey, 2) DASH box development utilizing individual interviews, and 3) free living pilot trial including DASH box intervention to determine effects on cardiometabolic markers. Methods: F/V preferences indicated in 50 surveys supported conceptualization of six DASH boxes displayed during 15 interviews. Following, a 28-day open trial enrolled 21 participants (12 females, 9 males), collecting pre- and post- measurements of blood pressure (BP), weight, waist circumference, and skin carotenoid levels while receiving DASH boxes and diet education. Results: Participants prefer fresh F/V, use staple items to compliment F/V, and experience barriers (time, money, transportation) to accessing or using F/V. Significant improvements in systolic BP (mean difference of -4.1土7.8 mmHg, p=0.01), diastolic BP (-3.7土6.4 mmHg, p=0.004), and WC (-0.8土1.1 inches, p=0.003) were found post-intervention. Mean difference in weight (-1.2土4.8 pounds, p=0.26) and skin carotenoid levels (26.7土74.1, p=0.06) changed, however, results were not significant. Conclusions: This pilot study suggests medically-tailored DASH boxes may be an effective nutrition intervention for lowering BP and other risk factors for Hispanic/Latine individuals with HTN.
Abby Lohr, C2DREAM Pilot Grantee, Through the Lens, Immigrant Perspectives on Health in Southeast Minnesota: A Photovoice Study
Abstract: Introduction. Policy makers in the United States (US) may be unaware of immigrants’ health-related priorities due to barriers (e.g., language, voting restrictions, or exclusion from political parties). In response, Rochester Healthy Community Partnership (RHCP) collaborated with 14 Hispanic/Latino and Somali immigrant leaders in southeastern Minnesota and used Photovoice to document their health-related assets and needs. This article illustrates the thematic findings from the Photovoice workshops and discusses the leaders’ policy recommendations. Methods. In Fall 2023, RHCP trained leaders in photography and Photovoice during a five-session workshop. Each session included a photography lesson, group reflections, and instructions for the following session. After taking photos, the leaders reflected, discussed the issues revealed in their images, and developed policy recommendations. From March through September 2024, we exhibited the photographs and shared recommendations with policy makers. Guided by Public Health Critical Race Praxis and the National Institute for Minority Health and Health Disparities Research Framework, we used thematic analysis to analyze leaders’ reflections. Results. Three themes emerged: healthy choices, the importance of culture and community, and access to opportunity. Leaders want to expand healthy choices in southeastern Minnesota by growing community garden programming, protecting the environment, making healthy options accessible (e.g., nutritious foods in workplace cafeterias), and constructing an affordable gym with private exercise space for women. They highlighted the importance of integrating culture and community into youth education, access to culturally appropriate foods, and the need to address Islamophobia. Leaders wanted increased access to job opportunities, affordable housing, and healthcare. They saw these opportunities as vehicles for self-improvement but emphasized time management as key to success in the US. Conclusion. We want to ensure that immigrants have a voice in shaping policies that impact our health. Policy makers can leverage these findings by demonstrating they have heard and acted upon participants’ policy recommendations.
Laura Suarez Pardo, MD, Assistant Professor, Mayo Clinic, Cardiac distress in Latinx/Hispanic women with cardiovascular disease and risk factors: examining its prevalence and the role of discrimination and acculturation experiences
Abstract: Psychocardiology has advanced the understanding of the depression and cardiovascular disease (CVD) association, followed by numerous intervention studies target in depression in CVD patients. However, the study outcomes have not been encouraging, suggesting the role of other areas of psychological distress. To that end, the concept of 'cardiac distress' is emerging, which is a multidimensional psychosocial construct that affects patients' ability to follow recommendations and recover from CVD. Nonetheless, this work is new and has primarily studied non-Hispanic whites, limiting the generalizability of these findings to underrepresented minority groups. Objectives: (1) Investigate cardiac distress in Latinx/Latino/Hispanic (L/H) women with acute coronary syndrome and those with traditional CVD risk factors; (2) examine the impact cardiac distress has on health-related quality of life (QoL); and (3) explore the impact of acculturation experiences, familism, and discrimination. Methods: This is a cross-sectional survey-based study. It will assess demographic characteristics, mental and CVD history. There is no cardiac distress measure; therefore, it will be evaluated with the STOP-D (anxiety, depression, stress, anger, social support), Impact of Event Scale-Revised (trauma), and Maastricht Questionnaire (vital exhaustion). Other assessments include SF-12 (QoL), PHQ-15 (somatic burden), EOD/EDS (discrimination), BASH and HSI-2 (acculturation), and the Familism Scale. Data analyses will include summary statistics for sociodemographics and cardiac distress prevalence, in addition to logistic regression for the relationship between cardiac distress, QoL, discrimination, acculturation, and familism. Conclusion: The study will investigate cardiac distress on L/H women with CVD, the impact of these conditions on QoL, and the role discrimination, acculturation, and familism have on mental and cardiovascular health. This study will be the first to address these objectives. The results may increase awareness about cardiac distress, be an opportunity to decrease healthcare disparities, and provide data that can assist in developing culturally sensitive interventions to improve psychiatric and cardiovascular outcomes.
Kate Diaz Vickery, Hennepin Healthcare Research Institute/C2DREAM, Co-investigator, Community Engagement CoreHeart health, wellness, and homelessness: Early open trial results of CV-HOMES
Abstract: People who have experienced homelessness (PEH) die decades sooner than their housed peers. Heart disease is the leading cause of chronic disease death among this population. PEH in MN have 3x higher death due to heart disease than the general MN population. We conducted design and feasibility research to create the Cardiovascular risk homeless support (CV-HOMES) program. CV-HOMES offers behavioral activation based wellness coaching to improve multiple health behaviors for PEH. We report on results from an early phase open trial with N=7 participants. We found CV-HOMES to be highly acceptable but found site-specific recruitment challenges which limited feasibility. The Lifes Essential 8 cardiovascular health score (0-100) was feasible but had notable challenges including the length of time it took to collect and the interpretability of the nutrition instrument in our population. We plan for a larger pilot randomized trial with a revised recruitment strategy to continue to develop CV-HOMES.
Erin Westfall, Mayo Clinic, Program Director, Mohamed Ibrahim, Putting Community Partners in the Driver's Seat: Insights from the Development of a Community-Based Participatory Research Framework Aimed at Reducing Cardiovascular Disease Disparities
Abstract: Context: Minnesota has the largest population of Somali immigrants and refugees in the U.S., and their rates of hypertension are growing. This is troublesome, as racial disparities in hypertension prevalence and control are observed nationwide. Community-based participatory research (CBPR) approaches have proven efficacious for investigating health disparities in minoritized populations by empowering communities, promoting understanding of culturally relevant issues, and addressing barriers to health. A rural MN community expressed a need and interest in developing interventions to address cardiovascular disparities. Objective: To improve the cardiovascular health of Somali Community members through concurrent development of the GMHEP, a CBPR framework, and research agenda. Study Design: This is a formative study. In 2021, our institution partnered with 3 community organizations (Public Health, SNAP, and WellShare International) to address health disparities of minoritized populations in rural MN through CBPR, with initial focus on hypertension in the Somali Community. Population Studied: Community partners. Intervention: The GMHEP partners collaboratively developed the mission/vision/values and operating norms of the partnership. GMHEP partners identified cardiovascular disease disparities as an area of concern and developed an intervention to engage Somali leaders and community members in hypertension prevention and self-management. A Somali partner completed research subjects training to recruit and consent participants for the study. Shortly after beginning recruitment of participants for the research intervention, the study was paused in observance of Ramadan. Research activities resumed after Ramadan concluded. Outcome Measure: GMHEP partner satisfaction. Results: GMHEP partners expressed high levels of trust and confidence in the research activities of the partnership, and team objectives, communication, and climate improved from 2021 to 2023. Development of partnership provided an avenue for community members to have concerns addressed; what strategies worked and what needs improved. Conclusion: When working within communities, it is important to be aware of the cultural and religious needs of the community partners and defer to their expertise on how and when to conduct research, even if this may delay the research process. Doing so builds trust between academic and community partners and is a critical step in the development of a CBPR framework LEARNINGOBJECTIVES: 1. To recognize the importance of engaging community in the study of health disparities. 2. To describe the process of embracing cultural humility and utilizing collaborative, equitable principles to drive partnership building in the development of a CBPR framework for a rural community.
-
Patrick Hammett, UMN: Center for Chronic Disease Reduction and Equity Promotion Across Minnesota (C2DREAM), Early Stage or Pilot Investigator, An Organizational Strategy for Reducing Tobacco-Related Cardiovascular Disease Risk among BIPOC Clients at Behavioral Health Clinics in Minnesota
Abstract: Commercial tobacco use is a leading cause of cardiovascular disease (CVD) and related chronic conditions (RCC) in the US, contributing to one of every four deaths from CVD. Compared to White individuals, Black, Indigenous, and People Of Color (BIPOC) individuals are less likely to utilize evidence-based tobacco treatments and experience higher rates of tobacco-related CVD and RCCs. BIPOC communities, particularly those in socioeconomically disadvantaged areas, also experience high rates of mental illness and substance use disorders (MI/SUD). Individuals with MI/SUD conditions have 2-3x the smoking prevalence of the general population, and smoking is the primary cause of excess mortality among individuals with serious mental illnesses. One strategy to increase the equitable delivery of tobacco treatment is to provide MI/SUD clinics with the training and resources they need to implement tobacco treatment protocols into their existing services. The primary objective of the present study is to conduct a community-informed pilot evaluation of the PLC program which provides behavioral health clinics with mentorship, coaching, and resources to integrate a tobacco treatment protocol into their standard treatment practices. This work seeks to address several extant gaps in the literature. First, it will evaluate the preliminary utility of the PLC program in a "safety net" MI/SUD clinic, which experiences additional barriers to tobacco treatment delivery including a lack of time, resources, and care fragmentation. Second, it will explore the equity impact of the PLC program by evaluating it separately within BIPOC and non-BIPOC patients. This will include an exploration of the roles that structural and social determinants of health play in affecting treatment delivery. Dr. Hammett has assembled an interdisciplinary research team whose training and mentorship will help ensure the successful completion of the project. This research will inform a future intervention effectiveness (R01) or intervention development grant (R34).
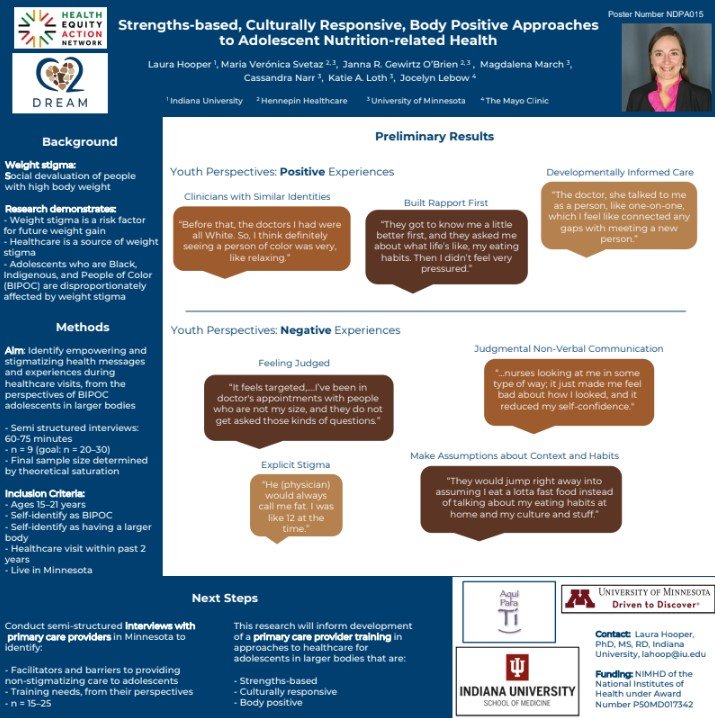
Laura Hooper, Indiana University School of Medicine, Assistant Professor of Pediatrics - Division of Adolescent Medicine Strengths-based Culturally Responsive, Body Positive Approaches to Adolescent Nutrition-related Health
Abstract: Weight stigma is a widespread problem based on social devaluation of people with high body weight. Accumulating evidence demonstrates that (1) weight stigma is a risk factor for future weight gain and healthcare visits are sources of weight stigma. BIPOC adolescents with high weight status are disproportionately affected by weight stigma and thus the focus of this study. To improve understanding of weight stigmatizing experiences at healthcare visits we are conducting semi-structured interviews to achieve the following aim: characterize empowering and stigmatizing health messages and experiences during healthcare visits, from the perspectives of BIPOC adolescents with high weight status in Minnesota. Youth identified the following positive experiences during healthcare visits: clinicians with similar identities (e.g., “Before that, the doctors I had were all White. So, I think definitely seeing a person of color was very, like relaxing.”), developmentally informed care, and build rapport first (e.g., “They got to know me a little better first…Then I didn’t feel very pressured”). Negative experiences youth identified included judgmental non-verbal communication, explicit stigma (e.g., “He (physician) would always call me fat. I was like 12 at the time”), feeling judged, and making assumptions about context and habits (e.g., “They would jump right into assuming that I eat a lotta fast food”). Results from this study will inform development of a primary care provider training in strengths-based, culturally responsive, body-positive adolescent healthcare. Long-term goals are to decrease weight stigma experienced by BIPOC adolescents during healthcare visits, thus contributing to improved cardiometabolic health in Minnesotan BIPOC populations.n text goes here
Warren McKinney Hennepin Healthcare Research Institute, Vice President of Equity in Research Cardiovascular Disease and Inactive Status: A Single Center Pilot to Evaluate Racial Disparities in Access to Kidney Transplantation After Waitlisting
Abstract: Background: Patients with end stage kidney disease (ESKD) are at increased risk of cardiovascular disease (CVD) and CVD-related death. Kidney transplantation offers ESKD patients improved outcomes when compared to dialysis, however persistent disparities exist that limit African American patients’ access to transplantation. CVD status is also significant to transplantation as patients with ESKD are required to complete cardiac stress testing and additional social screening to become eligible for transplant. Unmanaged CVD and exposure to negative social determinants of health (SDOH) (e.g. financial, housing, nutritional, and transportation instability) can prevent a patient from becoming eligible for transplant, or active on the waiting list. Active patients who experience a CVD event or a SDOH stressor may be made “inactive” and unable to receive a transplant until the clinical or SDOH stressor is resolved. Therefore, it is necessary to reduce inactive time to improve access to kidney transplant for African Americans and patients with low socioeconomic status. Approach: We will complete a retrospective chart review to evaluate the association between 1) CVD evaluation and inactive status; and 2) SDOH and inactive status among patients on the waiting list at a transplant center in a Midwest urban center. We hypothesize that 1) delays in CVD evaluation while on the waiting list is associated with longer periods of inactive time; 2) exposure to SDOH risk factors while on the waiting list produce longer periods of inactive time; and 3) that African American candidates accumulate greater amounts of inactive time because of less timely CVD evaluation and exposure to SDOH risk factors. Future Directions: This project will provide critical data to inform a community health worker-based intervention to reduce periods of inactivity among African American patients through timely CVD management and responses to social stressors.
Guillaume Onyeaghala, Opportunities to improve health outcomes for African Americans across Cardiovascular Disease and End Stage Kidney Disease.
Abstract: Background: Kidney transplant is the optimal therapy for end-stage renal disease in terms of patient survival, prevalence of cardiovascular disease (CVD), and cost. However, racial barriers compound donor kidney scarcity and disproportionately affect African American (AA) patients' access to living or deceased donor kidney transplants (DDKT). Despite this intervention, CVD will eventually occur or worsen in 54% of kidney transplant recipients (KTRs). AA KTRs should maintain good kidney function to minimize risk of CVD outcomes, which are among the highest in the state. KTRs must take a critical immunosuppressant, mycophenolate mofetil (MMF), to prevent kidney rejection. However, the gut microbiome may impact MMF drug metabolism, and social determinants of health (SDOHs) such as nutrition instability impact the microbiome. Therefore, SDOHs and the microbiome may be associated with clinical outcomes in AA KTRs. However, AA KTRs are often underrepresented in microbiome studies. In addition to factors involved in access to DDKT, it is critical we also identify barriers to their participation in microbiome research. Approach: Leveraging our community partnerships with the MN Links and SoLaHmo, our combined C2DREAM projects will examine 1) the impact of CVD on AA KTRs access to DDKT using a retrospective analysis and 2) community benefits for AA KTRs to participating in microbiome studies using focus groups. Future Directions: We established collaborations with local community partners to develop strategies informing our pilot work at Hennepin Healthcare. This will provide strategies aimed at reducing waitlist inactive time for AA KTRs and develop more community awareness for microbiome studies.
Francine M. Overcash, University of Minnesota, Postdoctoral Associate Barriers and Facilitators to the Mediterranean Diet Reported by Hispanic/Latinx Adults
Abstract: Little is known about the Mediterranean-style diet pattern impact among most racial/minority groups in the U.S, especially among the Hispanic/Latinx population, who may greatly benefit from the diet's established protective effects against CVD and Type 2 diabetes mellitus. The current proposal's long-term goal is to extend knowledge of CVD and T2DM prevention among Hispanic/Latinx adults in the Twin Cities by providing pilot data for a culturally tailored intervention aimed to promote a Mediterranean-style diet pattern. The innovation of proposed intervention lies in its design to capitalize on a hypothesized synergy between the Hispanic/Latinx culture and social network intervention principles. Hispanic/Latinx cultures are highly relational where family and kinship is paramount. Historically, interventions use non-network groups where the groups are comprised of individuals who have the same condition, illness, or life event and meet each other for the first time in the program. The established social circles paired with the shared experiences of the program will organically lead to more opportunities to practice the behavior modifications post intervention, thus leading to sustained behavior change. The current proposal offers both researchers and community stakeholders a tangible and prescriptive intervention design element with potential for wide-spread benefit to improving diet quality among Hispanics/Latinx that in turn may reduce CVD and T2DM risk.
Jeremy Van't Hof, Examining Urban and Rural Pharmacy Availability in Minnesota from 2009 to 2020
Abstract: Hypertension is a leading risk factor for cardiovascular disease in the United States, yet hypertension control remains poor and disparities exist by race and ethnicity. Despite many pharmacologic options for lowering blood pressure, medication access and adherence may be one cause for this health inequity. Much of the past research evaluating medication access has focused on cost as the primary factor for nonadherence, but geographic location is now being recognized as a possible determinant. Where one lives is influenced by a history of structural racism that limited who could buy a house and live in certain neighborhoods. By limiting access to certain neighborhoods, access to resources including healthcare may be limited. Neighborhoods with reduced access to pharmacies, "pharmacy deserts", have been described in several large cities. However, the location of pharmacy deserts in the Minneapolis-St. Paul metropolitan area (Twin Cities) is unknown. The overarching hypothesis for this study is that pharmacy access is more difficult for racially and ethnically minorized adults leading to reduced medication access and adherence. This inequity leads to worse hypertension control and increased risk for cardiovascular disease. To evaluate this hypothesis, we aim to identify pharmacy deserts in the Twin Cities using several methods to determine pharmacy accessibility for a neighborhood including travel distance, travel time, and proximity of a pharmacy to commuting routes. We will evaluate differences in desert and non-desert neighborhoods by race, income, and other social determinants of health to better understand factors that may be associated with a desert. In future research, we will use electronic health record data to evaluate average blood pressure in desert and non-desert neighborhoods. With this information and input from community stakeholders, we will design an intervention to improve hypertension control by modifying pharmacy access.
-
Junia de Brito, UMN: Center for Chronic Disease Reduction and Equity Promotion Across Minnesota (C2DREAM), Early Stage or Pilot InvestigatorUplifting Equitable Park Use and Promoting Physical Activity among African American Families in Minnesota: The NatureUplift Randomized Pilot Trial
Background: Physical activity (PA) and cardiovascular health disparities persist due to the inequitable distribution of resources and opportunities across neighborhoods. This particularly affects African American adults and children, who experience lower PA levels because of limited access to safe neighborhood green spaces (e.g., parks), stemming from historical disinvestment and discriminatory policies. Insufficient PA significantly contributes to cardiovascular disease (CVD) and related chronic conditions. Addressing these disparities is crucial for advancing cardiovascular health equity. In partnership with the community engagement team of French Regional Park, a suburban park within the Three Rivers Park District System (TRPD), this study aims to investigate the effects of a nature-based curriculum—with and without a hiking component—on physical activity, mental health, and blood pressure outcomes among African American parents and children living in Minnesota. Methods: The NatureUplift study is a two-arm pilot randomized trial aimed at evaluating the effects of a nature-based curriculum on moderate- and vigorous-intensity PA, mental health outcomes (perceived stress, positive and negative affect, and symptoms of depression and anxiety), and systolic and diastolic blood pressure among African American parent-child dyads. Thirteen parent-child dyads have been enrolled in the study. The study includes two intervention groups: NatureUplift+Active (active intervention group) and NatureUplift (delayed intervention group). Culturally-representative interventionists lead both groups. Both groups will undergo a 12-week NatureUplift curriculum consisting of light-intensity activities (e.g., outdoor yoga and forest bathing). The NatureUplift+Active group will additionally participate in a weekly moderate- to vigorous-intensity hiking activity. The delayed intervention group (NatureUplift) will engage only in the nature-based curriculum during these 12 weeks. Afterward, the delayed intervention group will undergo a shortened protocol for NatureUplift+Active program for an additional 4 weeks (16 weeks total). Outcome measures will be assessed at four time points: baseline, 4 weeks (process outcome), 12 weeks (primary endpoint), and 16 weeks (maintenance outcomes). These measures include objectively measured physical activity and blood pressure, as well as self-reported mental health outcomes using validated surveys. Results: We expect participants assigned to both study conditions to report improved health outcomes following exposure to nature-based programming. At the 12-week primary endpoint, we expect those assigned to the NatureUplift+Active intervention, relative to those assigned to NatureUplift only, will report greater improvements in weekly minutes of moderate- and vigorous-intensity PA, mental health, and blood pressure outcomes. Conclusions: The findings of this study have the potential to advance equity and environmental justice by demonstrating community-engaged and culturally representative approaches to involving African American families in health-promoting activities within suburban green spaces. This study will add to the growing body of evidence in green space research and inform more inclusive planning and policy changes that ensure equitable access and use of urban/suburban parks. Ultimately, this work can reduce health disparities and foster community well-being.
Ebiere Okah, UMN: Center for Chronic Disease Reduction and Equity Promotion Across Minnesota (C2DREAM), Early Stage or Pilot InvestigatorCommunication Behaviors Perceived as Biased by Hypertensive Black Patients
Abstract: Clinician stereotyping, a form of bias, significantly contributes to poor hypertension control among Black Americans, thereby exacerbating cardiovascular disparities. Traditional methods to address bias have proven largely ineffective. Thus, a novel approach is required to reduce Black patients' experiences of stereotyping. Patients encounter stereotyping through both what they hear and how they are treated. Therefore, an intervention designed to limit the transmission of racial stereotypes and decrease biased communication behaviors, informed by the experiences of Black patients, holds the potential to reduce the frequency with which Black patients feel stereotyped.
Our research entails focus group interviews with Black patients who have hypertension to identify and contextualize stereotypes and communication behaviors they associate with biased treatment. These findings will inform the creation of a concise pre-visit patient questionnaire aimed at addressing commonly stereotyped factors. This tool will enhance clinicians' awareness of patient-specific aspects, thereby reducing instances where Black patients feel judged solely based on their group membership. In the subsequent phase, these findings will be used to develop communication skills training for clinicians, with the aim of reducing behaviors that Black patients associate with stereotyping. Our study objectives are to (1) identify stereotypes and specific biased communication behaviors and (2) collaborate with community partners to develop a brief pre-visit questionnaire addressing factors at risk of stereotyping.
The overarching goal of this research is to enhance interactions with Black patients by fostering encounters in which they feel treated as unique individuals rather than representatives of their racial group. This approach will result in improved healthcare experiences for Black patients, greater engagement in care, and a reduction in disparities related to hypertension.
Samuel Savitz, Mayo Clinic, Evaluation of the Association of Area-based Deprivation Indices with Cardiovascular Disease Outcomes Across Racial and Ethnic Minority Groups in Southeast Minnesota
Abstract: Area-based measures for social determinants of health (SDoH) are increasingly being used to conduct research on health equities and prioritize resources for underserved communities. Area-based deprivation indices measure deprivation at the neighborhood level and communities with high area-level deprivation tend to have worse access to health care providers and greater exposure to environmental pollution. Area-based deprivation is also a major driver of health disparities in cardiovascular disease by race and ethnicity since individuals who are a racial or ethnic minority are more likely to live in areas with high area-level deprivation due to structural racism and residential segregation.
Despite the value of area-based deprivation indices, challenges remain in identified the best performing index for particular contexts. There are many indices with little comparative data on their relative performance. Additionally, these indices were developed with little or no input from individuals living in more deprived neighborhoods. The study will address these gaps through a mixture of quantitative and qualitative analysis. Aim 1: Compare area-based deprivation indices in the strength of associations with blood pressure and diabetes control and evaluate whether the strength of associations varies by race and ethnicity. We will quantify the association of the two indices with cardiovascular outcomes and assess interaction effects by race and ethnicity using medical records data for individuals living in Southeast Minnesota. Aim 2: Ascertain communitystakeholder perspectives on key measures for area-based deprivation. We will conduct two focus groups with diverse community members and solicit feedback on additional component measures that relate to area-based deprivation.
This study will provide critical evidence that will inform the selection of an area-based index for studying and addressing cardiovascular health inequities in Minnesota. This work will lead to a larger grant to optimize the best-performing index and add additional component measures identified in the focus groups.
Amy Noser, Social Determinants of Health and Pediatric Type 2 Diabetes Management
Abstract: Pediatric type 2 diabetes (T2D) disproportionately affects individuals identifying as Black, Indigenous, People of Color (BIPOC). Social determinants of health (SDOH) contribute to health disparities in T2D prevalence among racially and ethnically diverse individuals.Objective(s): Describe C2Dream pilot study methods and present baseline demographics and SDOH of the current sample. Methods: Phase 1 includes assessment of SDOH via baseline measures. In addition, ecological momentary assessment (EMA) surveys, accelerometers, and electronic pill caps are used to capture real-time assessments of treatment adherence, diabetes management behaviors, and associated SDOH-related barriers. Phase 2 of the study will involve partnering with communityorganization, Appetite for Change, to conduct caregiver-youth focus groups to inform development and refinement of an adherence-promotion intervention for youth with T2D. Results: Thirteen youth (15.1±1.9 years old; 61.5% assigned female at birth) have completed Phase 1. The racial and ethnic background of youth included 23.1% Asian American, 15.4% Black or African American, 7.7% White, and 38.4% Multiracial, and 15.4% not reported and 15.4% Hispanic. Thirty-one percent of families reported that they received food support or food stamps and 61.5% of youth received free or reduced meals at school. On average, youth reported low to medium levels of perceived safety and exposure to violence in their neighborhoods. Conclusions: Youth with T2D come from diverse backgrounds and encounter SDOH that may influence their diabetes management behaviors. Interventions designed to meet the unique needs of this patient population are essential.
Antonio Paniagua Guzman, University of Minnesota Medical School, Postdoctoral AssociateThe Impact of Colonization on Indigenous Cardiovascular Health in Minnesota: Developing a Conceptual Framework
Abstract: Indigenous health disparities are rooted in multiple colonization practices such as war, genocide, racism, displacement, environmental destruction, and assimilation. In the United States, Indigenous populations have been disproportionately impacted by cardiovascular disease (CVD) and related chronic conditions (RCC). This population has higher proportions of premature death by CVD and RCC compared to the general population, and based on current patterns, this disparity appears likely to keep growing. Previous studies have focused on understanding the impact of mental health, sociocultural, and behavioral factors contributing to this pattern. Most of these works have largely drawn on macro-level, aggregated, quantitative data, without considering the culture, context, and uniqueness of every Indigenouscommunity. There is a dearth of culturally safe micro- and meso-level qualitative research on Indigenousunderstandings and conceptualizations of the impact of colonization on Indigenouscardiovascular health. In Minnesota, this represents a barrier for the development of research and interventions aimed at addressing current CVD and RCC disparities in Indigenouscommunities. Using a community-based participatory research framework in partnership with the Fond du Lac Band of Lake Superior Chippewa (Ojibwe) based in northern Minnesota, this pilot study will utilize semi-structured interviews and sequential focus groups to accomplish two aims: (1) Compare and analyze how older Indigenous people (age 55+) living with CVD and/or an RCC and younger Indigenous people (age 18-40) with an RCC that elevates their risk for CVD conceptualize the impacts of colonization on CVD risk, treatment, and outcomes. (2) Develop a conceptualframework based on Indigenous lived experiences to effectively guide future projects and interventions aimed at addressing CVD/RCC inequities in Minnesota Indigenous communities. This project takes an innovative approach to addressing health inequities in a marginalized population in northern Minnesota that have not previously been explored and will provide a conceptualframework to shape future programming and research.
Mary Whipple, UMN: Center for Chronic Disease Reduction and Equity Promotion Across Minnesota (C2DREAM), Early Stage or Pilot InvestigatorThe Transformative Impact of an Advisory Board in a Community-Based Study: Interrupt Type 2 Diabetes
Abstract: Type 2 diabetes (T2D) and its associated cardiovascular complications disproportionately affect African (Black) Americans. As a result, preventing or delaying the development of T2D and its associatedcomplications is essential. We sought to develop a community-engaged partnership in North Minneapolis, a historically Black neighborhood, focused on understanding how Black people age 55 and older experience T2D and how interrupting sitting time could be integrated into their daily lives. The purpose of this abstract is to describe the collaboration between community stakeholders and university faculty and students that led to the (re)development and funding of the Interrupt T2D Study. To ensure the voices of Black older people with T2D cocreated the study activities, we established a Community Advisory Board (CAB) of 4 community stakeholders (community members 55 and older who identify as Black, several of whom have T2D). We held our first meeting in August 2023 to discuss the original application and plans for revision. As a result, we re-designed the project, greatly simplifying the study, reducing the work required of participants, and ensuring we centered the voices of Black older adults with T2D. The project was ultimately funded and is actively recruiting participants from the North Minneapolis community represented by our CAB. Since the project began, the CAB has been integral to our progress, leveraging their knowledge and networks to expand community partnerships to include churches, the YMCA, and neighborhood initiatives; supervising data collection; and guiding dissemination. Ultimately, our monthly CAB meetings provide in-depth insights into the history of the North Minneapolis community – its buildings, spaces, and people, greatly enriching the study, our collaborative partnership, and the potential impact in a community of people who bear the greatest burden of T2D.
ESIs and Pilot Scholars presented at the poster session during the 2024 HEAN Annual Meeting in San Francisco.
Poster Gallery: